Gaps in Nigeria’s Flawed Model for Universal Health Coverage
February 2021
In Canada, when a teenager needs to get an immunization or a bandaid we usually just go to a school nurse or a family clinic. They’re very easy to reach and use, especially if you live in an urban area. You can almost always trust your doctor or nurse to give you the appropriate treatment you need and give qualified health advice.
Unfortunately, this is rarely the case for developing countries. In developing countries, the budget, prioritization, and social support around a highly functional healthcare system is often very low.
A solution that many developing nations are exploring is a health system called primary healthcare (PHC). Basically, building health posts and repurposing houses to deliver basic health services (e.g. immunization or a bandaid) with high patient satisfaction and financial viability. In doing so, the coverage of health services can be affordably and effectively maximized across an entire country.
The idea isn’t to be as sophisticated as the tax-funded healthcare system in Canada — just to provide basic health services to everyone who needs it.
Nigeria is one of dozens of countries with a PHC system. Considering their high rates of disastrous health outcomes, like maternal and child mortality, an effective PHC model could be revolutionary in improving the lives of their citizens.
Background on Nigeria + the health of their citizens
Crash Course on Nigeria
For context, Nigeria is one of the poorest and most populous countries in the world. 70% of their population lives on less than $1 USD a day, and ~50% of people live in rural areas (where poverty is most common).

Illiteracy is tragically common, with a literacy rate of 61.3%. Women are affected most; 72.1% of men are literate, whereas only 50.4% of women are.
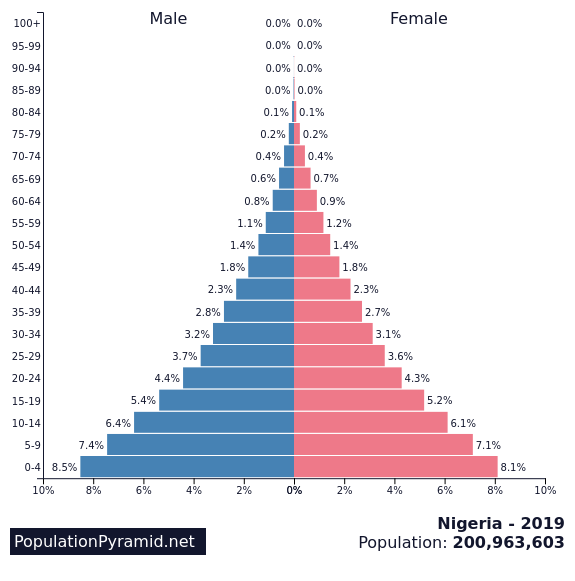
The population is largely made up of young people, with 0–14 year-olds representing the bulk of all citizens. The next most common age demographics are 25–54 years and 15–24 years.
What does this mean for their healthcare?
Nigeria’s slow urbanization and high poverty rates mean that accessible health services need to be highly affordable and within reach of rural areas.
The commonality of illiteracy (Canada’s is 99%) implies that medical advice and communication of health outcomes to patients needs to be non-written, especially for women.
Also, because most people are young, a successful health system needs to have an increased provision of child/adolescent services to be useful for the majority of the population.
So… why do healthcare quality and access need improvement in Nigeria?
Answer: catastrophic rates of poor health outcomes.
The health of citizens of developing countries tends to be lower than those of developed ones. Relative to Africa, Nigeria is one of the nations that face this problem at the greatest magnitude.
- maternal mortality ratio → 576/100 000 live births
- under-five mortality rate → 128/1000 live births
- infant mortality rate → 69/1000 live births
- only ~25% of children are fully vaccinated. 21% aren’t vaccinated at all.
Global standard:
- maternal mortality ratio → 211/100 000
The main causes of mortality and morbidity (suffering from disease) in Nigeria are vaccine-preventable diseases, infections, parasitic diseases, malaria, diarrhea, acute respiratory infections, and malnutrition.
What’s worse: the country ranks #187 out of 197 countries in the world in health system efficiency with respect to spending on health per capita (🚨 ). Nigeria likely wouldn’t have such deep health problems if it had a robust and effective system for improving health (healthcare).

These factors contribute to an average life expectancy of 54.33 years (as of 2018). In comparison, the UK’s is 81.26 years (~150% higher). This is clearly a huge problem, which a strengthened healthcare system could solve.
PHC is the first step in improving these health outcomes.
Children and mothers are dying, Nigerians aren’t living long enough, and disease is rampant. Half of the population lives in rural areas, and most of the population lives on <$1 USD daily.
It’s evident that to solve this problem, we need a healthcare framework to effectively improve health outcomes, while being highly accessible and highly affordable. This is the goal of PHC in Nigeria.
Unfortunately, less than 20% of potential patients utilize PHC services in Nigeria.
Less than 47% of pregnant women give birth in PHC centers. 25% of pregnant women give birth in-home, even with PHC centers relatively closeby. To contrast, in the US (2017), 61/62 (98.4%) births took place in hospitals.
98.4% compared to <47%. There’s clearly a problem with Nigeria’s PHC system.
While the goal for PHC as a viable healthcare strategy exists, its quality and access are extremely inhibited because of several factors. As a result, citizens don’t feel incentivized to use their services.
However, if PHC could solve its key barriers and problems (I’ll discuss these later), it could be a viable mode of healthcare for the majority of the population → increasing health coverage in the process.
Let’s dive deeper Nigeria’s current PHC system
Primary healthcare is the most basic form of healthcare provided in Nigeria, designed to be the first point of contact for non-specialized health advice and treatment (like a family doctor). The functions of primary healthcare are the promotion of health, early diagnosis of disability and disease, and the prevention of disease.
PHC services are delivered through PHC facilities, which includes health posts/clinics, health centers, and comprehensive healthcare centers. A PHC facility looks like a mobile or static structure where different health services are provided by groups of different kinds of health workers (doctors, nurses, midwives, etc.). Services can also be implemented through home visits.
Vitamin A supplementation, immunizations, maternal care services (prenatal, birth deliveries, antenatal), child care services, prevention and treatment of communicable diseases, public health education, family planning, environmental health, malnutrition management, and health data collection are services expected of PHC facilities.

Secondary (SHC) and tertiary healthcare (THC) also exist → they’re basically more advanced and specialized forms of healthcare that are catered towards urban areas. If a PHC facility patient requires more specialized or advanced treatment, ideally a referral can be made. Basically, the patient will be transported to an SHC or THC hospital. Most PHC facilities lack the infrastructure to provide safe and effective referrals.
Governance of PHC + its place in the national health system
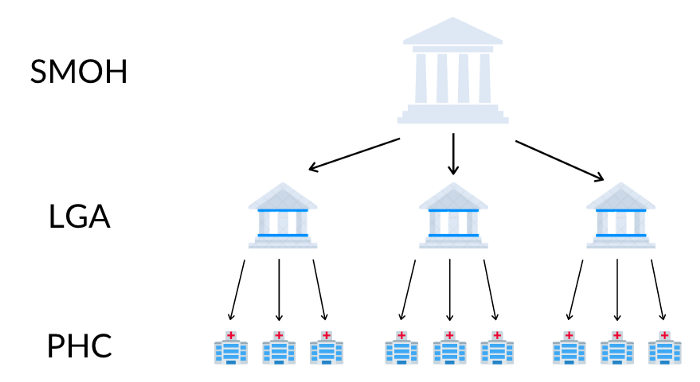
In Nigeria, the government is organized into 3 tiers → federal, state, and local government area (LGA). Each plays a different role in monitoring and managing the health system, particularly for primary healthcare. There are 36 states, each with their own LGAs.
Each state has a ministry of health (SMOH) and each LGA has a local health department. PHC facilities can be owned by the government, private for-profit organizations, or private-not-for-profit organizations.
Private sector facilities also deliver PHC services and are typically positioned in urban areas exclusively.
In the public sector, LGA health departments are responsible (owning + funding) the PHC facilities within their areas. SMOHs support and oversee the PHC activities of LGAs as a whole, while the role of an LGA is more granular → directly supervising the activities of each of its PHC facilities.
All tiers of the government strengthen health and management programs implemented in PHC systems through mechanisms like direct secondment of staff (temporarily reassigning staff for support), organizational support and technical support. Development partners (ex. WHO, world bank) assist states with improving PHC delivery. The federal government also creates and implements policies involving PHC.
This is a very simplified explanation → several more structures exist in monitoring and managing PHC. A key problem here is that the roles each of these actors play in the management of PHC as a whole is very unclear. Overlap of responsibilities and tasks is very common.
How is PHC financed?
Healthcare as a whole in Nigeria is financed through sources like tax revenue, out-of-pocket payments from households, international donor funding and health insurance.
Government spending on healthcare, particularly for PHC, has decreased over the past decade and isn’t enough to support PHC facilities. The proportion of the federal ministry of health’s (FMOH) budget for PHC activities went from 8.4% in 2012 to 4.7% in 2015. As a result, out-of-pocket expenditure is the biggest piece of total health expenditure (69.35% in 2013).
A lack of sufficient government funding is a key driver for poor PHC outcomes, like a lack of essential medicines in-stock or delayed/non-existent salary payments for health personnel.
Federal Financing
The FMOH budget towards PHC includes funding for health programs (ex. the national immunization program, the rollback malaria initiative) and constructing PHC facilities in LGAs. The amount currently budgeted towards PHC inadequate.
Sometimes all of the money allocated isn’t released, even when the funds are needed. For example, in 2011, the total federal-level capital budget allocation for health was ₦63.4B. However, only ₦38.8B was released (61.2%), and just ₦26.02B was utilized (67%).
State Financing
States also allocate budgets for healthcare, but the way they spend them doesn’t make sense. The issue of budgets not being released exists at this level as well. This leads to poor implementation of health program activities (because of a lack of funds).
LGA Financing
Funds for PHC come here through a variety of different channels, but they’re mostly financed from federal government revenues.
LGAs are the main source of financing of PHC facilities. They provide staff salaries, money for facility construction + maintenance, drug supply, equipment, and other medical commodities. For healthcare programs like immunization, federal and state governments provide logistical and financial assistance.
However, due to a lack of established rules/policies on how this should work, it’s unclear if any meaningful financial assistance does come from states and how it’s coordinated with LGA budgets for PHC. Generally, accountability and transparency about the management of finances for healthcare are extremely weak.
LGAs also budget money towards healthcare, but financial allocations don’t extend far beyond paying the salaries of health workers. Not much is left for developing health programs that would be implemented in PHC facilities.
Also, the proportion of state and LGA budgets allocated to the health sector is below 15%. Less than 3% of Nigerians have some form of insurance coverage.
Not enough is being financed towards healthcare (especially PHC), and budgets are highly mismanaged. Other sources of funding (ex. development partners) contribute to programs and PHC infrastructure, but out-of-pocket spending is the leading method of financing.
This is problematic for those who, likely in rural areas, don’t have money to spend on healthcare and have no insurance coverage. What’s worse: even if impoverished Nigerians are able to pay for health services, having to do so traps them in poverty because of how much health costs take out of their already small earnings (<$1 USD/day).
Because of poor management, accountability, and transparency around PHC financing, health personnel at PHC facilities often encounter delays with salary payments. Along with other causes, this is why there’s inadequate availability of human resources for health.
Human resources for health are suffering from weak PHC financing.
Human resources for health (HRH) = the main workers at the PHC level. In any PHC facility, this could include community extension health workers (CHEWs, people from communities who undergo training to assist their community’s PHC system), community health assistances, community health officers, doctors, nurses, midwives, lab staff, and/or public health nurses. The majority in PHC are CHEWs, while doctors, nurses, and midwives are more available in other levels of healthcare.
Unfortunately, the availability of health personnel is extremely low in Nigeria. For a population of 1000, there are an estimated 0.403 physicians, 1.605 nurses and 0.137 chews. This is especially a problem at the PHC level, where many facilities are often run by 1–2 nurses max.
As an example: in Enugu state, there are 0.31 medical doctors on average per PHC facility, compared to 195.5 for tertiary (more advanced) hospitals.
To put that into perspective:
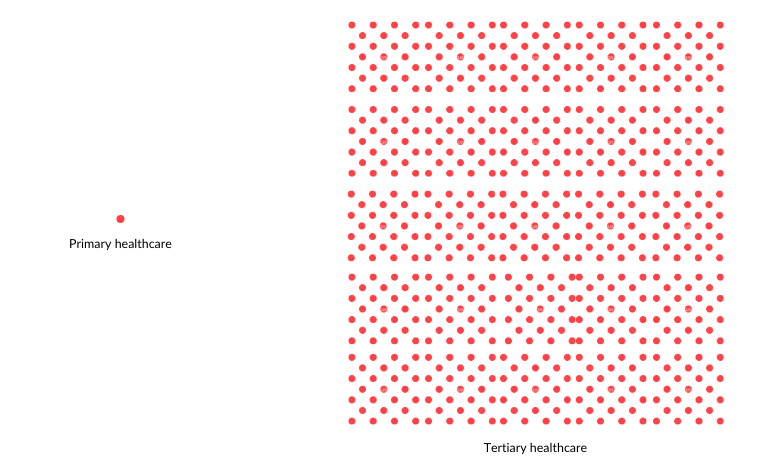
You can imagine it’s difficult to deliver high-quality healthcare if there aren’t qualified people to do so.
But what does “qualified people” actually look like in terms of health personnel?
Basically, most health workers that go on to work at PHC undergo 2 years of training in a classroom environment. They gain little insight into what it’s like to work at a real facility, leading to difficulties fulfilling their roles once actually stationed in a health center. That’s if you’re lucky enough
to
find work after training (which not everyone is).
Training support is also provided and recommended to PHC professionals that already work in facilities. This process is also flawed; those who actually need training support usually aren’t those who actually get it, leading to staff demotivation and attrition. The availability of training resources and supports also varies heavily across states and LGAs.
For those who do receive training, a gap between what they’re taught and how they actually perform exists. For example, CHEWs often don’t do the community practice that’s expected of them.

This is caused by:
- a lack of clarity and understanding around their roles
- poor staffing (not enough HRH, not enough of certain roles), resulting in workers having to do roles they weren’t trained to do (ex. CHEWs doing the work of midwives)
- negative organizational culture and attitude at PHC facilities (leading to general underperformance)
Regulatory and monitoring processes exist as quality inspection mechanisms to circumvent this, and maximize the performance of HRH in PHC centers. Unfortunately, most of the systems and structures in place to do this aren’t effective enough because of poor accountability + transparency, poor planning, and a lack of government-led established strategies.
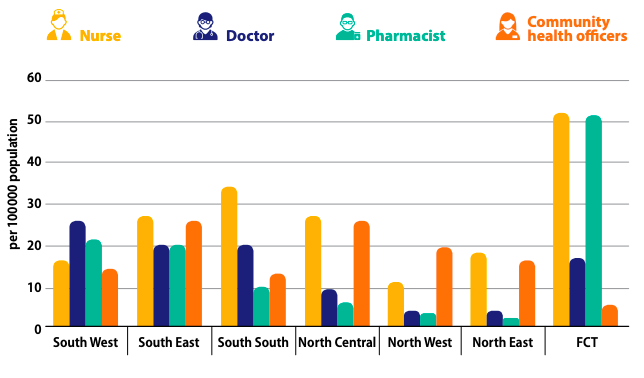
Aside from poor training, unavailability of HRH, and a lack of effective monitoring, other problems with health personnel exist at the PHC level. Imbalances in skill ranges and large disparities in HRH distribution between rural and urban areas are tragically common.
Not only does Nigeria lack enough health personnel to deliver PHC services to everyone, but the amount available varies heavily across rural and urban zones and private/public PHC facilities.
Attraction and retention of HRH in rural centers are very low. Those looking to work in PHC tend to bias towards urban facilities, resulting in a personnel deficit for rural ones. Workers who are stationed at rural facilities often feel demotivated. This is because rural life is perceived as difficult, and their PHC facilities tend to be of lower quality.
Rural areas having poorer PHC facilities is one of the reasons why their inhabitants tend to have more disastrous health outcomes than urban areas, but social determinants of health also play a large role. For example, poor living conditions, mass poverty, and other common concerns in less developed regions of Nigeria. To tackle this, more collaboration between the health sector and other governmental sectors are necessary.
Rural PHC workers have to operate in centers with a lack of basic amenities (ex. electricity and water), less personnel and equipment, an inadequate supply of drugs, and are usually separated from their families who don’t live in the area. Low job satisfaction and low staff performance are direct outcomes, leading to high staff turnover.
If I had to work in a facility with the accommodations of a decaying abandoned warehouse, I probably wouldn’t like it either.
Northwest and northeast regions of Nigeria are especially under-resourced with doctors (where poverty and illiteracy are more common). Also, only 12% of practicing doctors work in public/private PHC.
The way health personnel are currently governed (in terms of policy) also contributes to their demotivation and turnover. A lack of prioritization in terms of policy creation and adherence is partly responsible for why issues with HRH still exist to such a great extent.
Zero (out of 774) LGAs have sufficient policies or plans for managing HRH, so efforts aren’t being coordinated to address the clear problems with health workers. The National Human Resources for Health Policy was created for all government tiers to use as a starting point for HRH management, but less than 50% of states actively use them. Until accountability is taken at the governmental level and appropriate steps are taken, system-wide issues with health personnel will be difficult to solve.
Regulation + Accountability
To bolster accountability and transparency within the health system and to regulate its activities, a mix of government/development partner-led and community-led approaches are currently being used.
Government-/Development Partner- Led
“PHC under one roof” is a model that the federal ministry of health and development partners use as guidance to states for improving PHC service delivery. It basically aims to achieve centralization of management; integrating all PHC services under one authority. By doing this, supervising and monitoring systems for facilities and referral mechanisms between integrated facilities would be much easier. However, implementation attempts have been very weak. Standard treatment protocols and job aids are also given to primary care teams to guide them in diagnoses and providing appropriate treatment for minor illnesses. Specific guidance is given concerning treating common conditions a CHW could see while working within PHC. However, most CHWs don’t use aids when attending to patients for ‘personal reasons’, potentially because of a lack of appropriate enforcement mechanisms. This is the equivalent of trying to build a chair without reading the instruction manual… inefficient and easily leads to failure.
At the state level, healthcare providers have policies and guidelines for regulating medicines provided and quality of health services. State ministries of health are especially responsible for the latter.
Several professional regulatory bodies exist for maintaining and regulating standards of training and practice for HRH. However, they aren’t very effective — they’re limited by weak structures and a low ability to set and meet goals concerning healthcare. They can’t carry out important functions or effectively monitor and accredit training institution programs. The priority of regulating HRH is there but such structures for doing so are highly ineffective.
What’s worse — even if these flawed structures could effectively identify malpractice in the health system, actually enforcing regulations is challenging. Health workers have been found disobeying regulations, overstepping boundaries, and worse — but avoid penalties when caught.
TLDR: we have structures in place at the government/professional level for regulating PHC-level activities, but regulation processes have low efficacy and enforcement in practice.
Community-Led
Community participation is a super important aspect of primary healthcare. By assigning a degree of authority to communities where PHC facilities are located, their utilization and satisfaction of PHC services should increase. Thus, regulatory structures for primary healthcare also exist at a less formal, community-based level.
They’re called “village health committees”, where community representatives speak on behalf of citizens about health service planning and evaluation. They monitor the work of PHC facilities and support them through community health volunteers. These committees were designed to maximize community participation and act as accountability structures. Specifically, they hold PHC accountable for its management of finances, service delivery performance, and political engagement.

Unfortunately, like with governmental regulatory structures, a variety of factors are preventing them from effectively regulating primary healthcare. They lack the technical and managerial skills to be effective external accountability structures. Additionally, committee members are offered zero incentives and are unclear on who to report to.
Monitoring and evaluation go hand in hand with regulation and accountability. To improve the PHC system, the ability to monitor and regulate its activities and outcomes to identify and address problems is crucial.
Monitoring and Evaluation
Monitoring and evaluation = monitoring the activities of PHC and evaluating their outcomes (to identify areas of improvement + track progress).
PHC facilities report monthly to their LGA, and the LGA reports to their SMOH. Specific departments in a SMOH collects routine health information from the community and facility level through LGAs and sends this to the federal level database.
What’s “reported” is how PHC facilities are meeting a set of 48 healthcare indicators. This data is used to assess the quality of health centers across Nigeria. Some categories of indicators are health policy, health status, social + economic indicators, and provision + utilization of health services indicators.
However, the process of managing this information isn’t strong enough because of challenges with data governance, data quality, and the use of information. It has the potential to be much stronger and viable for the health system, but despite significant investments made, the system is very weak. Plus, we know that this is directly harming the quality of care offered at PHC centers. When supportive supervision and teamwork between states and health facilities is maximized (through systems like monitoring), quality of care improves.
A key stemming issue for this is LGAs and states are often unable to deliver timely, reliable, and complete data. Data gathering is typically weak in most areas, because of:
- weak governance
- lack of commitment to duty
- inadequate funding and infrastructure
- low capacity
- shortage of personnel
- deficient skills in data management
- in PHC → poor capacity to collect, collate and analyze data
For the few states who do report in a timely manner with regular data collection from their LGAs, but actually analyzing this data and feedback for planning and improving health outcomes isn’t common yet. This is so dumb — basically, even if monitoring systems are working and useful data is being collected, it just isn’t being used for anything.
Because data can’t be gathered effectively or meaningfully used, a lack of data-based evidence exists in the process of making informed health planning and priority decisions. To contextualize how problematic this is — imagine having to choose a restaurant to go to without being able to read any reviews! You probably wouldn’t make the best decision because of a lack of information. For something like healthcare, making the wrong decisions can obviously result in disastrous outcomes.
Other Problems with Quality of Nigerian PHC
Ultimately, the goal is to maximize the utilization of PHC services. This is dependent on two main factors; high-quality health services with high accessibility. Without either, potential clients (especially in rural areas) won’t be incentivized or able to attend PHC facilities and receive adequate care.
It’s important to note that in recent years, Nigeria has improved the utilization of its PHC services. One of the biggest value propositions of PHC centers is maternal care, and the proportion of all births done by skilled birth attendants (mostly at these facilities) increased from 38.9% in 2008 to 58.6% in 2014. However, a huge inequity between utilization exists between rural and urban areas:
- urban areas → 79.2% of births assisted by trained personnel
- rural areas → 46.6% of births assisted by trained personnel
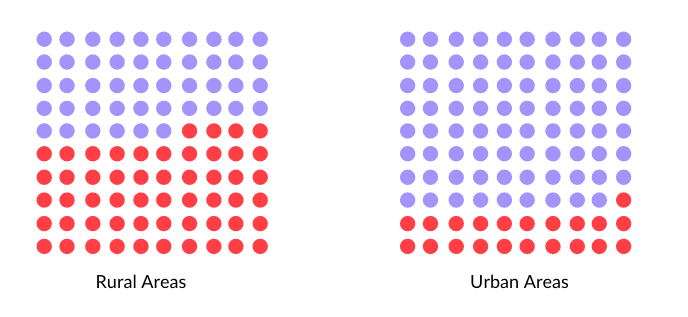
Similarly, the proportion of less than 1-year-olds immunized against measles (a service expected of PHC centers) increased from 2008 to 2014, but again, urban areas were the majority of those users. Knowing that rural PHC facilities tend to be of lower quality, this is a key reason as to why its usage in rural areas is lagging behind so much.
Some other causes + lower-level PHC quality issues as to why rural areas tend to be underserved:
- governmental factors (ex. lack of political commitment, inadequate funding/misappropriation of funds, weak intersectoral collaboration and intergovernmental struggles for power and control)
- people/client-related factors (ex. community perceptions of poor quality and inadequacy of available services in PHC centers, underutilization of PHC services, lower levels of community participation)
- lack of motivation in workplace (ex. because of poor remuneration)
- unhealthy rivalry between different categories of health workers
- non-involvement of private health sector in planning + implementation of PHC
- poor management of information systems
- heavy dependence on initiatives funded by foreign donors
Here are some problems (aside from what we’ve already discussed) with PHC quality:
Deficit in Provision of Community-Based Health Services from CHEWs
As community health extension workers, one of their major job responsibilities is to provide direct healthcare services to members of their communities. However, due to logistical challenges, very few to no CHEWs spend 80% of their time in their communities. This leads to weak community participation and ownership of health outcomes (which is the opposite of what the PHC system wants).
Lack of Equipment and Amenities and Poor Infrastructure
Most PHC facilities are poorly equipped. Only ~25% have more than 25% of the minimum equipment package. Just 20% of PHC facilities can provide basic obstetric services. You get the point.

Unfortunately, quality can be even worse if you live in certain regions. The competency and range of services provided vary heavily geographically and geopolitically. For example, 0.5% of PHC facilities in North-Eastern Nigeria provide immunization services, whereas 90% do in South-Western Nigeria.
The infrastructure of PHC centers themselves tends to be horrible, mostly because of a lack of necessary funding from state and local governments. Basic amenities are also largely unavailable — like electricity, emergency transportation systems, water, and healthy sanitary and waste management practices. I wouldn’t want to go to a clinic with lights that don’t turn on.
The availability of medical products is particularly problematic. Less than 50% of PHC facilities have essential drugs in stock, and even then, the authenticity and potency of drugs is a problem. 40% of them on the market (which PHC facility workers purchase) are found to be fake or substandard. There are several causes as to why this is → a lack of government commitment to managing the drug market, irregularities in the supply of products from local government stores to health facilities, and poor funding.

After LGAs pay for salaries of HRH at PHC facilities, little is left for medical products and equipment. Thus, PHC providers have been found to participate in illegal or sketchy medicine purchasing schemes to make ends meet.
Incorrect Disease Diagnosis
Partly because workers (ie CHEWs) don’t follow aids given for identify common diseases, incorrect diagnosis is very common. In 2012, only 37.4% of all cases of tracer diseases (ex. malaria) were correctly diagnosed by all health workers in PHC facilities.
Poor Links Between Levels of Care
Hospital referrals are difficult for PHC facilities to provide because of challenges of access and mobility from the initiating (PHC) facility to the receiving (more high-end) facility. There’s also no reporting system for the success of a referral if a referral actually goes through. Communication between levels of care in the referral process is extremely weak; zero follow-up or feedback from the receiving facility or patient is the norm.
Corruption within the health system
In a report by Gavi, it was found that $2.2M USD had been misused within the health sector by Nigerian officials… and refunded to them. The issue of corruption is wide ranging with tons of different actors, like senior/junior admin officers in health ministries, health personnel and agencies.
Interestingly, corruption can be directly linked to quality of healthcare provided → it’s been estimated that a 10% increase in corruption = 10–20% reduce in immunization rates.
The primary causes for why this still exists (despite being a priority for political leadership) is a lack of transparency and adherence to law within the health sector, and how the public sector is ruled by ineffective civil service codes with weak accountability mechanisms.
Lack of clarity around responsibility of local governments for PHC
Local governments are expected to be the main implementers of PHC policies and programs, but the constitution makes it unclear whether states are expected to be more responsible for PHC delivery. Sometimes, this leads to confusion in roles and responsibilities of those governing PHC, and weaker management = weaker quality of care.
It’s pretty clear that there are a ton of problems and respective causes for why PHC facilities aren’t meeting expectations for quality of care. From the citizen perspective, barriers of accessibility are also deterrents from utilizing primary healthcare services.
Problems with Nigerian PHC Access
Women have enormous influence over their communities and their usage of health services. If the women see a PHC facility as excellent and love its services, the community as a whole will use the PHC facility. Additionally, these health centres concentrate most on providing maternal and child care services (which, culturally, women take almost complete responsibility of).
Therefore, when understanding why residents of a community don’t attend a PHC facility, it’s important to specifically focus on why women don’t → everything depends on their reasons and experiences. Women in rural areas face the most problems with accessibility and motivation to use PHC, and here’s why:
Physical Accessibility Factors
PHC centers are far and hard to get to for pregnancy care, especially if you don’t own a motorcycle (the majority of people in rural communities). Very unappealing.
The major constraint on transportation is poor roads. Especially when PHC facilities are outside of short walking distance, poor road networks (hard to navigate, non-motorable) prevent rural Nigerians are a massive obstacle. In the event of heavy rainfall or undeveloped road infrastructure, people are trapped inside their communities and are forced to default to traditional birth attendants (TBAs, people who assist with births without formal training) or elders for pregnancy delivery.

In fact, roads can be so bad that they can cause miscarriages when trying to transport pregnant women to PHC facilities. Not a risk I think many would want to take.
Even if road networks aren’t particularly horrible, if you don’t have a motorcycle (the most common vehicle), having to walk long distances for health services is extremely demotivating — especially in cases of emergency. Lots of communities don’t have a PHC facility nearby (despite a strong want), and so giving birth at home is considered the next best option.
Facilities also aren’t always open, and citizens are often uncertain as to whether a health worker is present and available to care for clients. Hours of operation are usually just 10am-2pm. Adding to this, nurses are known to abandon centers to go to the market or other places.
If you had to travel long distances over poor roads without a car, without even knowing if the center is open, just for a chance at low-quality health services… you probably wouldn’t feel all that encouraged to use PHC either.
Perceptions of Poor Quality of Care @ PHC
Women in rural areas would rather give birth at home than at a PHC center. They see very little value from the services provided by facilities. This is largely because of how HRH behave (remembering how they’re demotivated to work in rural communities and have low accountability/transparency mechanisms).
Provider competence is generally perceived to be poor → citizens, especially women, aren’t confident in the people working at PHC facilities. Some workers can’t even recognize signs of labor in women, and waiting times are extremely high (often with no good reason). As such, it’s a custom to not go to PHC centers and instead visit TBAs or elders, who are thought of as more experienced and helpful.
Health workers are also known to be unfriendly and deceptive. As you probably know, pregnant women are super emotional and moody during labor. They’ve said that nurses can make them feel worse → by shouting at them, not giving them proper care, and generally not being nice people. Sometimes they’re even borderline scammy, adding in informal charges to patients, suggesting inappropriate referrals to make them pay more, and completely not caring for patients. In some areas, nurses are known to pressure patients into purchasing drugs they need to buy at ridiculous margins.
It gets worse. The amount of providers at centers usually isn’t enough, and for those who are there, unavailability to serve clients is painfully common. It’s hard to find a real doctor at a facility, who patients view as a necessity for high quality of care. Nurses are usually present, but sometimes, aren’t around on weekends or only are present in late hours. The issue of inadequate staffing is perceived as one of the biggest detractors from using PHC.
Cost of Care
The direct cost of care of using PHC services is another barrier. The price is seen as high for a government hospital — people would rather pay less for a private hospital, even if that means paying more for transport.
example direct costs of care at different facilities:
- ₦10,000 (US$27.8), ₦12000 (US$33.3), ₦8000 (US$22.2)
“Why our women are not using this PHC centre is because the price is high and it is a government hospital, when our women give birth here, they are charged Naira10,000 (US$27.8), Naira12000 (US$33.3), Naira8000 (US$22.2). But if we go to Bode hospital [secondary facility] we will pay the transport, but it will be cheaper, that is why they don’t come to this PHC” (source)
- “Any small sickness they will charge ₦3000 (US$8.3), ₦4000 (US$11.1) but in general hospital, it is ₦500 (US$1.4), ₦1000 (US$2.8)” (source)
From the perspective of rural inhabitants, PHC centres need to know direct costs are too high so that they’re lowered. Malpractice is also suspected on behalf of PHC because of how high costs are, and what the government initially should’ve set them to be. However, direct cost of care isn’t seen as the biggest barrier and some think the prices charged are reasonable.
That being said, TBA pricing is known to be much more flexible and much cheaper. Considering the other downsides of PHC centers, TBAs are seen as the better option. This is because, even if costs of care objectively aren’t that high, rural citizens likely still can’t pay them. Considering 70% of Nigerians live on less than $1 USD daily, it’s difficult to find a price that’s viable for a PHC facility while accomodating all patient needs.
Husband Support
In Nigerian culture, husbands support their pregnant wives in various ways. A lack of support can prevent pregnant women from being able to use PHC services. This could be in terms of money, or even assistance in domestic chores like caring for children. Although, sometimes, men give women money to go to PHC clinics → but there’s the possibility that it isn’t enough to match the cost of care.
Misinterpretation of Signs of Pregnancy Complications
Lastly, it’s not impossible that women don’t realize they have pregnancy complications and falsely think they don’t need the help of a PHC to give birth.
All of these factors multiply against one another in dissuading rural women from using PHC for health services over local alternatives, thus causing a community-wide distrust in the PHC system. To tackle this problem and promote the utilization of primary healthcare services, such key barriers with quality and access need to be addressed and solved.

There’s no reason why accessing health services as simple as a pill bottle or diapers should be impossible, anywhere. Child mortality, maternal mortality, and widespread disease could all be mitigated with better health coverage.